mRNA vaccines
What they are:
A new tool for the job
Your immune system’s job is to recognize foreign bacteria and viruses and clear them from your body. Your immune system does this using antibodies. Antibodies are large proteins created by immune cells that recognize and bind to a piece of a foreign invader, such as a virus. This process helps your immune system detect the infection and clear it from the body. When a virus infects you, your body needs to identify that the virus is foreign, develop antibodies that recognize it, and ramp up antibody production to mount a full defense. But this process takes time. It’s usually during this span of time, starting when an infection has taken hold in your body and ending when your defense mechanisms have cleared out the virus from your system, that you feel sick.
Vaccines work by giving your immune system a head start. Most vaccines expose your immune system to a weakened or nonfunctional virus or viral parts, so your immune system learns to recognize that virus and develops antibodies for future use. If you later become infected with that virus, your body will have already developed the antibodies to fight it, and the virus will be defeated before you ever know you were infected.
A virus is made up of two fundamental parts: a nucleic acid genome, either made of RNA or DNA, and an outer coat, made of protein and often lipids. Traditional vaccines present your body with portions of that outer viral coat so your immune system can produce antibodies to recognize that virus. mRNA vaccines take a different approach. Instead of delivering the viral outer coat to your immune system, mRNA vaccines deliver a portion of the viral genome and allow your own cell’s machinery to make the viral proteins that your immune system will learn to recognize.
How it works:
Using your cells to make viral proteins
Cells synthesize proteins through a two-step process: transcription—copying DNA into RNA—, and translation—reading the RNA to make proteins. Most RNA viruses hijack this second step, translation, by injecting their genetic material into your cells and having the cell’s ribosomes produce all the proteins needed to make new viral particles that will go on to infect more of your cells. mRNA vaccines take a page out of the virus playbook and use the body’s cells to produce fragments of viral proteins. These parts are insufficient to make new viruses, but are enough to instruct the immune system to make antibodies to fight the virus.
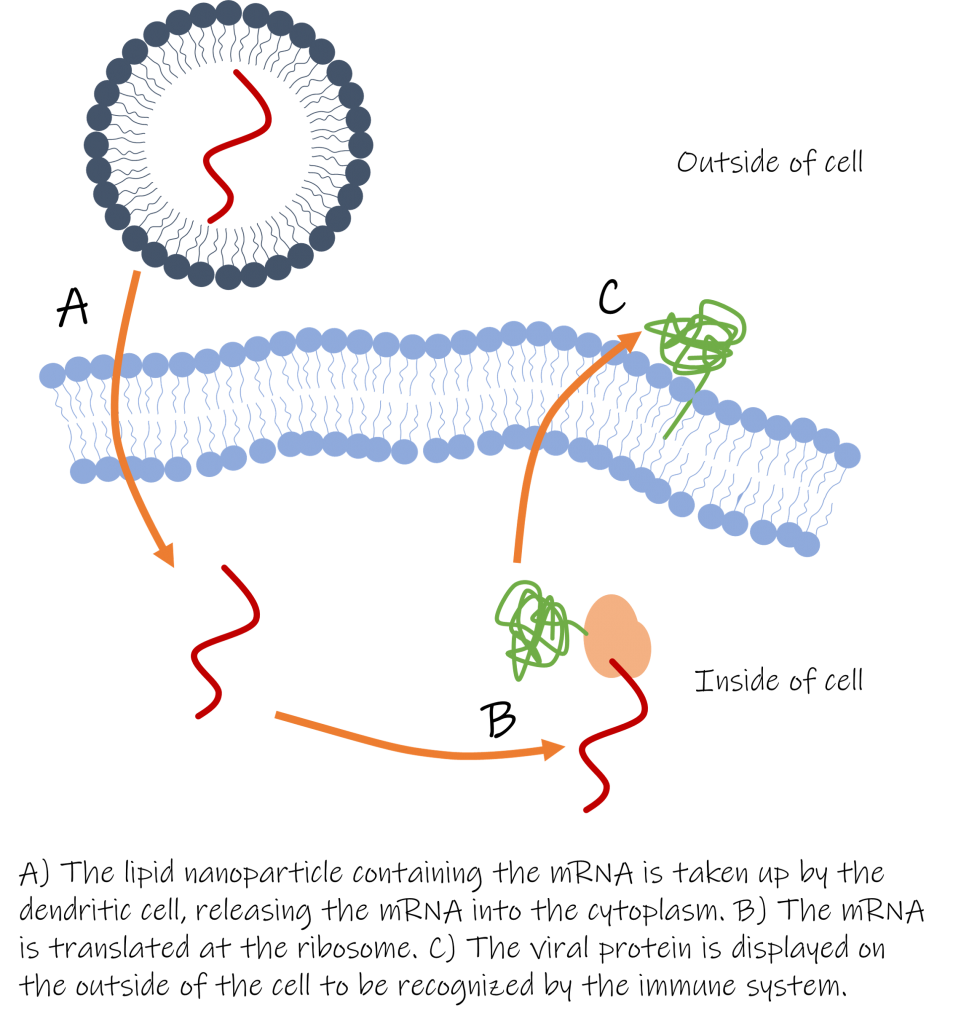
To develop an mRNA vaccine, scientists select a viral protein that will trigger the development of effective antibodies. They then design the mRNA that, when translated, will produce a harmless part of the selected viral protein. To help the mRNA get into our cells, it is packaged in an outer coat of lipids, making what is known as a lipid nanoparticle. This is necessary because mRNA is a large negatively charged molecule, meaning it can’t easily cross the cell membrane, and also because the body has enzymes that quickly destroy most mRNAs found outside of a cell.
After receiving an mRNA vaccine, the lipid nanoparticles are taken up by the immune system’s dendritic cells, which gather foreign particles and signal the immune system to develop an immune response. When the lipid nanoparticle is taken in by the dendritic cell, the mRNA is released and translated by the ribosome. The protein is then transported to the dendritic cell’s outer membrane, where the immune system will recognize it as foreign and develop an immune response. If the same virus later infects you, the immune system will already have antibodies to fight and defeat the infection, before you ever knew you were sick.
The benefits:
Safe, quick to develop, and leading the way for new treatments
One advantage of mRNA vaccines is that they are expected to be very safe. The vaccine contains no virus, viral particles, or anything that could ever be contagious. It only contains the instructions for making a single (or even just part of a single) viral protein. Furthermore, the mRNA is short lived, and is naturally degraded shortly after translation.
mRNA vaccine production can also be faster and more cost-effective than traditional vaccine production. In the COVID-19 pandemic, mRNA vaccines were administered to humans on a large scale for the first time. From the discovery of the SARS-CoV-2 genetic sequence to the first clinical trial of a new vaccine took only 66 days—a new record. Scientists believe the process could be even faster in the future. The key is that when new mRNA vaccines are made, scientists can switch in a new mRNA coding sequence from the new virus, leaving the rest of the vaccine unchanged. In contrast, traditional vaccines often require a much more intensive development process that can often take years. Scientists hope that new mRNA vaccine development could be measured in days. Many scientists think we should even develop mRNA vaccines for potentially dangerous diseases that haven’t ever infected humans—yet. Imagine if scientists had developed vaccines for SARS-like diseases before the first person was infected with SARS-CoV-2.
With vaccines leading the way in delivering mRNA to cells, new doors could also open for treating other diseases. Delivering mRNA or other large molecules to cells has long been proposed to treat many diseases. A major difficulty lies in getting those large molecules into the cells. While RNA vaccines were not the first treatments to use lipid nanoparticles as a drug delivery device, their development has advanced the science around their use. Now, with widely used and profitable vaccines driving the science, treatments for other less common diseases may also benefit from these advances.
Questions
Review:
- How do antibodies help our immune systems fight infections?
- How do traditional vaccines make your immune system more effective at fighting a virus in the future?
- For an mRNA vaccine, where is the viral protein that your body will recognize actually produced?
- Why is it necessary for mRNA to be delivered by a lipid nanoparticle?
- What is one reason it could be easier to design new mRNA vaccines compared to traditional vaccines?
Critical thinking:
- In the cell, DNA is used to code for mRNA and then mRNA is translated into protein. One of the drawbacks of mRNA vaccines is that the mRNA is not very stable at room temperature. But DNA is very stable at room temperature. Nucleic acids delivered using nanoparticles only enter the cytoplasm. Knowing this, would a DNA-based vaccine delivered using nanoparticles work? Why or why not?
- An mRNA virus is made of two parts: the mRNA and the lipid nanoparticle shell. Compare and contrast this structure with the structure of a virus.
Discussion:
- Some scientists think we should be spending time and money developing vaccines for diseases that may in the future become pandemics, so that we are ready when they come. Other scientists think time and money is better spent on working on vaccines for very rare diseases that infect humans currently. If you were in charge of distributing money to vaccine researchers, who would you be more likely to give money to, someone studying a disease that may (or may not) become a pandemic, or someone studying rare diseases that people currently are infected with?
Answer key:
Available to teachers upon request: dnadots@minipcr.com
